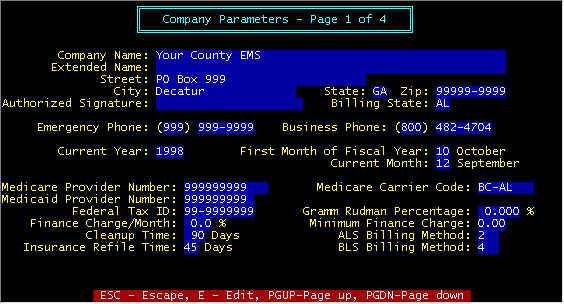
Screen 1 - Insurance Refile Time -- This specifies the number of days that allows
Medicare/Medicaid/Insurance claims to be refiled (only via forms-not electronic), and is
the number of days past due. In other words if the field contains 30, then after the claim
is 30 days past due, refiles will be enabled, and when refiled claims are selected from
the PRINT/FORMS/REFILES menu chain, then claims that qualify
will be printed (refiled).
Screen 1 - ALS/BLS Billing Method -- As defined by Medicare,
beginning January 1, 1995, New HCPCS codes will be optional until April 1, 1995, and
mandatory thereafter. There are 4 billing methods , and this may vary from carrier to
carrier. Consult with your carrier as to which method(s) are in use in your state. These
methods and HCPCS codes are elaborated in the section accessed via the menu selection MAINT/System Files/Supplies.
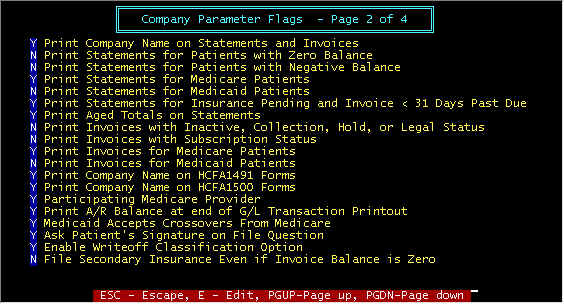
Screen 2 - Print Company Name on Statements and
Invoices -- N(o) if you are using pre-printed forms with your company name and
address.
Screen 2 - Print Statements for Patients with Zero Balance -- Print
statements for paid up accounts.
Screen 2 - Print Statements for Patients with Negative Balance -- There
is a patient report that list overpaid accounts. From this a check can be sent to the
patient, Medicare, Medicaid, Insurance Company that overpaid rather than send a statement.
Periodically, go to the PRINT/Patient List/Patients With
Negative Balance Invoices, and from this printed list reimburse the overpaid party, and
post a negative payment in the amount of the reimbursement so that the invoice will show
zero balance.
Screen 2 - Print Statements for Medicare/Medicaid Patients -- Per
preference of the EMS provider. It is recommended to print these for Medicare, but not
Medicaid so that when payment (in some cases Medicare copay) becomes the patient
responsibility, then prior statements shall have been received stating some thing to this
effect "We have filed with Medicare and awaiting payment – currently due from
you $0.00). You may not want a global lockout on sending
either a Medicare or Medicaid patient a statement by setting N(o) here, but may want
instead to individually prevent specific invoices to be included in statements. This
can be done by setting the invoice status to H(old). Note
that a rejection by either Medicare or Medicaid considers
that the invoice is no longer these payors, but becomes private pay at which time your
selection here is overridden.
Screen 2 - Print Statements for Insurance Pending and Invoice < 31
Days Past Due -- Per preference of the EMS provider to print statements not overdue
and insurance payment pending.
Screen 2 - Print Aged Totals on Statements -- Either print one
total due line or four lines plus total due line; the four lines are the due amounts
listed by time overdue (0-30 days, 0-60 days, etc.).
Screen 2 - Print Invoices with Inactive, Collection, .......... Status
-- normally not done
Screen 2 - Print Invoices with Subscription Status -- Invoices are
simply a notification of service, not necessarily a request to pay. This will
enable/disable notification of services for subscribed patients.
Screen 2 - Print Invoices for Medicare/Medicaid Patients -- normally
not done for Medicaid, normally done for Medicare. An invoice is not a request for payment
(except for private pay), but simply details of services performed, and is the only time a
patient receives a line item by line item listing of all charges. As with statements
(above) you may want to globally lock out printing invoices to
these payors, but do it on an individual basis.
Screen 2 - Print Company Name on HCFA 1491/1500 Forms -- Some forms
may already have your name and address printed.
Screen 2 - Participating Medicare Provider -- First, a definition
of what a participating provider entails, and then the pro's and con's of being one (and
this may vary from state to state, as well as locality-to-locality). To become a
participating provider requires that in November/December, proper application is made so
that the application can become effective beginning January 1st. This is binding for 12
months, and if it is desired not to participate, the following Nov/Dec, the application
must be made to get out. After becoming a participating provider, you must accept
assignment on all claims. Additionally, Medicare will crossover secondary insurance claims
via Medigap; approved Medigap codes must be included in the insurance company records.
This means that Medicare will file with secondary insurance companies for you. In some
states, Medicare automatically files with Medicaid for you, whether you are a
participating provider or not, and this may vary from state to state. One advantage of
being a participating provider is that Medicare checks are mailed to you. One disadvantage
is that you must accept the "Medicare Allowed" amount which may be considerably
less than your charges, and the difference between what is charged and what Medicare
"Allows" must be written of as a Medicare Contractual Writeoff, and by law is
uncollectable by any means. Medicare will pay 80% of the allowed amount, and it is your
responsibly (and obligation) to collect the remaining 20% from secondary co-pay sources
(insurance, Medicaid Private Pay, etc.). In non-participating cases, you can collect the
full amount from the patient, whereupon you file for them, but the check is mailed to the
patient. Whether or not being a participating provider is advantageous is strictly on a
case-by-case basis, and best determined by each provider. If you are in a locality with
more than one provider, you may be at a competitive disadvantage if the other provider is
participating and you are not, since the financial obligation may be less for the patient
using the participating provider. There is a HCFA mandate in the works that all
providers MUST be participating.
Screen 2 - Print A/R Balance at end of G/L Transaction Period -- At
the end of each transaction period (usually daily), G/L transactions are printed for
journal entry into an independent G/L system. The computed balance can either be printed
or not by the Y/N entry into this field, The down side of printing this balance is the
compute time required, but in most cases is not objectionable.
Screen 2 - Medicaid Accepts Crossovers From Medicare -- If Medicaid
is secondary to Medicare, in some states Medicare will file automatically with Medicaid
for you. If selected, the secondary date filed field in the invoice file will be
automatically set to the date filed with Medicare: ACCEPTED: Alabama, Florida, Georgia,
Mississippi, North Carolina, Tennessee. NOT ACCEPTED: Kentucky. Note that this is subject
to change, and you should check with Medicaid.
Screen 2 - Ask Signature On File Question if Medicare Paycode -- If
N(o), the phrase "Signature On File" will be printed on HCFA1491 forms, and the
Medicare paycode window in the invoice screen will not have this message and field. If
Y(es), this question is displayed each time a Medicare paycode is selected in an invoice
paycode window: Sign. On File Y/N
Screen 2 - Enable Writeoff Classification Option -- If N(o), All
writeoffs will have the same classification. If Y(es), the operator can classify writeoffs
when posting payments and these classifications are printed in the TRANSACTION LOG and
OPERATIONS report. Additionally, if Enabled, then you will have an adjusted collection
efficiency (bottom half of OPERATIONS report that gives you credit for contractual
writeoffs. Recommend enabling with Y(es).
Screen 2 - File Secondary Insurance Even if Invoice Balance is Zero -- Preference
of the EMS provider whether or not to file secondary insurance after the invoice has been
paid. Normally not done.
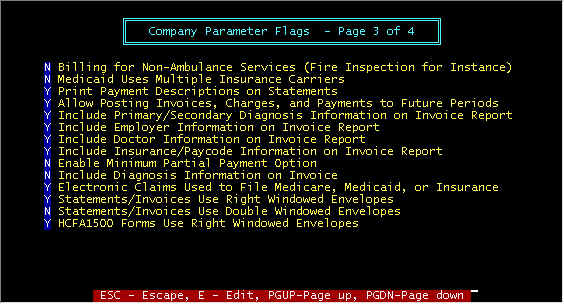
Screen 3 - Billing For Non-Ambulance Etc. -- A
separate company can be created to allow billing for Non-Ambulance services (fire
inspection, e.g.). Statement and Invoices will have no reference to patients.
Additionally, all services of this type must be on a separate company, not mixed with
normal EMS services.
Screen 3 - Medicaid Uses Multiple Insurance Carriers -- If this
flag is set to Y, the insurance company (carrier) code entry will be required when a
Medicaid paycode is entered (in the invoice), with subsequent data entries as though an
insurance company paycode had been entered. The insurance company name is printed at the
top of the HCFA1500 form. , with the only exception being when Medicaid is secondary to
Medicare. If MEDICAID IS SECONDARY TO MEDICARE, the insurance company code will not be
required, and this is the only exception. Only a few states are using multiple insurance
carriers for Medicaid claims; examples are Tennessee and Arizona.
Screen 3 - Print Payment Description on Statements -- When posting payments, a payment description can be entered, and if
this option is enabled here, this description will be printed on statements, and is
helpful for the patient to understand the statement. For example, the description next to
a Medicare payment may read "$100 deductible, $53.92 patient copay". With such a
message, the patient should understand why they owe $153.92. However, some patients do not
read, and thus use of a highlight pen is helpful to point out certain areas such as this
where you would like to attract their attention.
Screen 3 - Allow Posting Payments Invoices, Charges and Payments to
Future Periods -- If the month has not been closed and you are in the next month,
enabling here will allow entering/posting in a month that is future to the current period
(month). This will create accounting discrepancies (amounts) on statistical reports by
month, and is not recommended.
Screen 3 - Include ....................On
Invoice Report -- In the main invoice screen, the R-Report
option will print all information about the highlighted invoice so that this report can be
turned over to a collection agency, legal authorities, etc. Certain options here will
determine what data to exclude/include from this report.
Screen 3 - Enable Minimum Partial Payment Option -- For private pay
where a monthly payments have been established, a payment
lower than minimum will not be considered as adequate so as to eliminate past due
statements (see PAYCODE7 records per section Fi.9 (menu tree FILES/9-Paycode 7 Private
Pay).
Screen 3 - Include Diagnosis Information on Invoice – Normally
not done
Screen 3 - Electronic Claims Used to File Medicare, Medicaid or
Insurance – Y if either of these are electronic
Screen 3 - Statements/Invoices Use Right Windowed Envelopes – Y
= right window, N = left window
Screen 3 - Statements/Invoices Use Double Windowed Envelopes – Prints
both Mail-to and return addresses in windows
Screen 3 - HCFA1500 Forms Use Right Windowed Envelopes – The
mailing address will print on the left or right side (in the envelope window position)
depending upon your choice here. Y = right window, N = left window. Some vendors supply
laser forms with a bar code in the left window, and thus right windows are required.
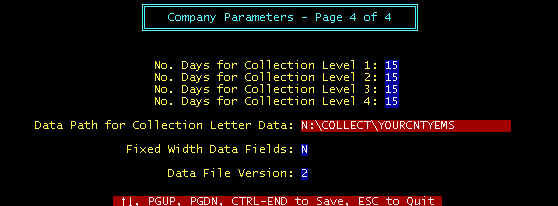
Screen 4 - No. Days for Collection Level 1 -- Extraction
of collection letters has programmable features. The number of
days is the elapsed time since the last letter was extracted before the next letter is
eligible for extraction. For example, 15 days (minimum) must lapse from the time
collection letter 1 is extracted before collection letter 2 is eligible for extraction;
then 20 days until collection letter 3, etc. The data path is simply the disk directory
where the collection data is stored. Select N(o) for word processor mail merging and
(Y)es) for EQUIFAX -- No=take out space-filled characters that could result in unwanted
spaces, between first name and last name, e.g.
Screen 4 - Data Path for Collection Letter -- Each time collection letters are extracted, the files LETTER1.DAT,
LETTER2.DAT, etc. are written to disk drive C, subdirectory COLLECT, with a series of
records, one for each patient, and each record has the data format as shown below. Note
that the drive and subdirectory can be specified, and the ones shown here are for example
only. If collection letter 1 is being extracted, the system erases the file
C:\COLLECT\LETTER1.DAT, and then rewrites a new C:\COLLECT\LETTER1.DAT (if any are
extracted), otherwise there will be no existing LETTER1.DAT. This ensures that specific
collections letters (letter 1, 2, etc.) are only sent one time.
Screen 4 - Fixed Width Data Fields – Yes for EQUIFAX, No for all other.
Screen 4 - Data File Version – As data the extracted data files are changed, added to, etc. as time goes on,
new data versions are generated so that users of data 1, 2, etc. who do not choose to
change to newer versions so as not to disrupt your current usage (word processors,
collection agencies, etc.) will not need to be changed.
Extraction Data Format for Collection Letters -- The different data
versions are discussed in more detail under the menu COLLECT.
Shown below is data version 2, for example:
"M1
-10002","MURPHYJS","10/22/92","John","S","Murphy","John","S","Murphy","Rt.
2, Box 231M","Green
Mountain","CA","62813-9523","(555)","555-1212","256-09-3044","193.00","0.00","193.00",
"Y"
Note that the computer converted from all CAPITAL (Upper Case) to Upper
and lower case-this is because collection letters do not look good in all CAPS. You may
recognize the data as: Invoice Number, Patient Code, Service date, Patient Name,
Responsible Party, Address, Phone, Social Security Number, Charges, Payments, Balance due.
Note that the N(o) option was chosen for the example. See Section D-Collect for more
details