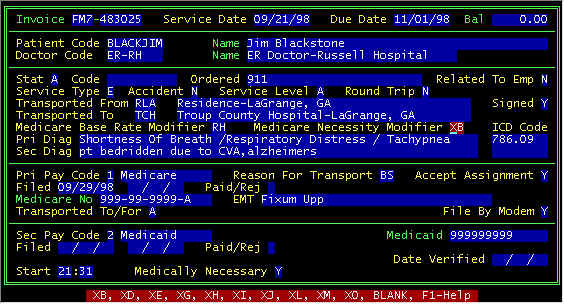
Screen 1--Kentucky Invoice Screen
Click here -> to return to the Table of Contents
Invoice Screen
Kentucky State-dependent Codes/Fields
SPECIAL STATE-DEPENDENT FIELDS IN THE INVOICE DATA ENTRY SCREEN
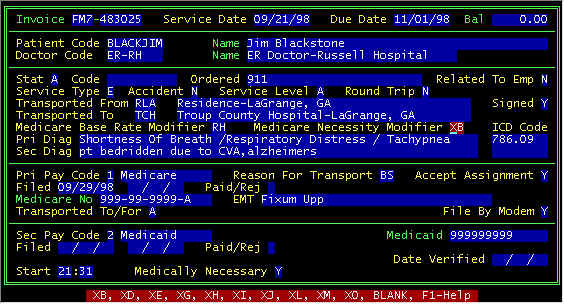
Screen 1--Kentucky Invoice Screen
The Kentucky invoice screen is the same as other states except for the Medicare Necessity Modifier only used in KY, and Paycode windows (Medicare and Medicaid) which vary from state to state. All fields that are not unique to KY are described here. The prompt line in screen 1 above shows the 2-character choices for the Medicare Necessity Modifier, and pressing the function key F1 displays the help screen shown below.
Screen 2--Kentucky Medicare Necessity Modifiers
ENTERING THE PRIMARY AND SECONDARY PAYERS IN THE INVOICE DATA ENTRY SCREEN
The system uses numbers 1-9 to designate the different type payers, these numbers we call paycodes. With time, knowing these paycodes will become second nature. However, at first, you may either need to write these down for reference, or use the help screen. When your cursor is at one of these paycode fields, pressing function key F1 will display the following:
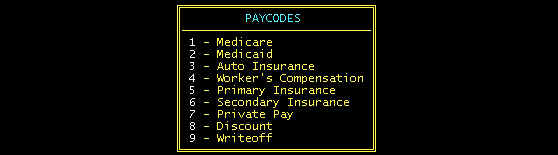
Screen 3--Paycode Choices
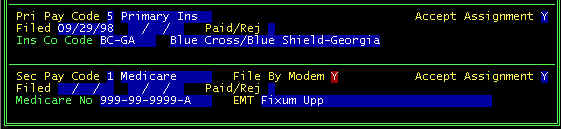
Medicare is the Primary Payer--Window in Invoice Screen--see screen 1 above
Reason for Transport --
Either enter none, 1, 2 characters per the prompt line at the bottom of the screen, or
press function key F1 for the help screen
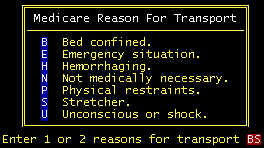
Reason For Transport Help Screen
The following are listed in the order of importance/severity: U, H, E, P/B, S, N.
Note that B is more important than S. always use B when possible, but be prepared to
specifically say why in the secondary diagnosis narrative. Leaving both characters blank
is acceptable, but not advisable.
Accept Assignment -- Participating Providers Must Accept Assignment. This means at least two things: (1) You must accept the Medicare Allowed Amount on the EOB as the total amount you can collect when there is a non-zero allowed amount. Medicare will pay 80% (if there is no deductible), and you are required to attempt to collect 20% from either secondary coverage (coinsurance) or from the patient (copay). (2) Payment comes directly to the ambulance company rather than to the patient.
Filed -- There are two dates, the first is for the first filing, and the second is the refile date.
Paid/Rej(ected) -- Automatically set when posting payments, but can be manually changed here.
Medicare No -- HIC number copied from the patient screen.
Transported To/For--The prompt line at the bottom of the page will display your (single letter) choices. Pressing the function key F1 will display the help screen below.
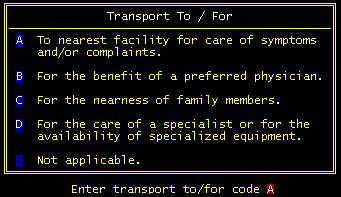
Transported To/For Help Screen
File By Modem - defaulted per the flag in the company screen parameter flags. If Y is in this default, then this will be defaulted here. However, there may be certain claims that need to be filed paper, even though electronic claims being used. If N appears here, this claim will not be extracted for electronic transmission.
Medicare
is the Secondary Payer--Window in Invoice Screen--about
the same as Medicare primary shown in screen 1 above.
Medicaid
is the Primary Payer
Window in Invoice Screen
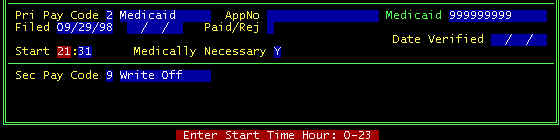
In the primary paycode window, when 2 is entered in the Pri Pay Code field, the top half of this window is displayed.
AppNo--Approval Number for
Non-Emergency transports
Medicaid--Medicaid number extracted from the patient file
Filed--two date fields, the first is first filing date, second field is the refile date
Paid/Rej--Automatically set to either P or R from posting payments, but can be overwritten here
Date Verified -- for your won usage--the date you verified eligibility--most often not used
Start Time--Hours and minutes in military time.
Medicaid
is the Secondary Payer
When Medicaid is the secondary payer, generally they will do what ever the primary does,
using the same charges, HCPCS codes, diagnoses, etc. The invoice window for Medicaid
secondary is shown above in screen 1, and the field descriptions
are the same as Medicaid Primary as described immediately above.